Benefits and Challenges of School-Based Teledentistry Programs

You can’t educate a child who isn’t healthy, and you can’t keep a child healthy who isn’t educated.
– Dr. Joycelyn Elders, former Surgeon General of the U.S.
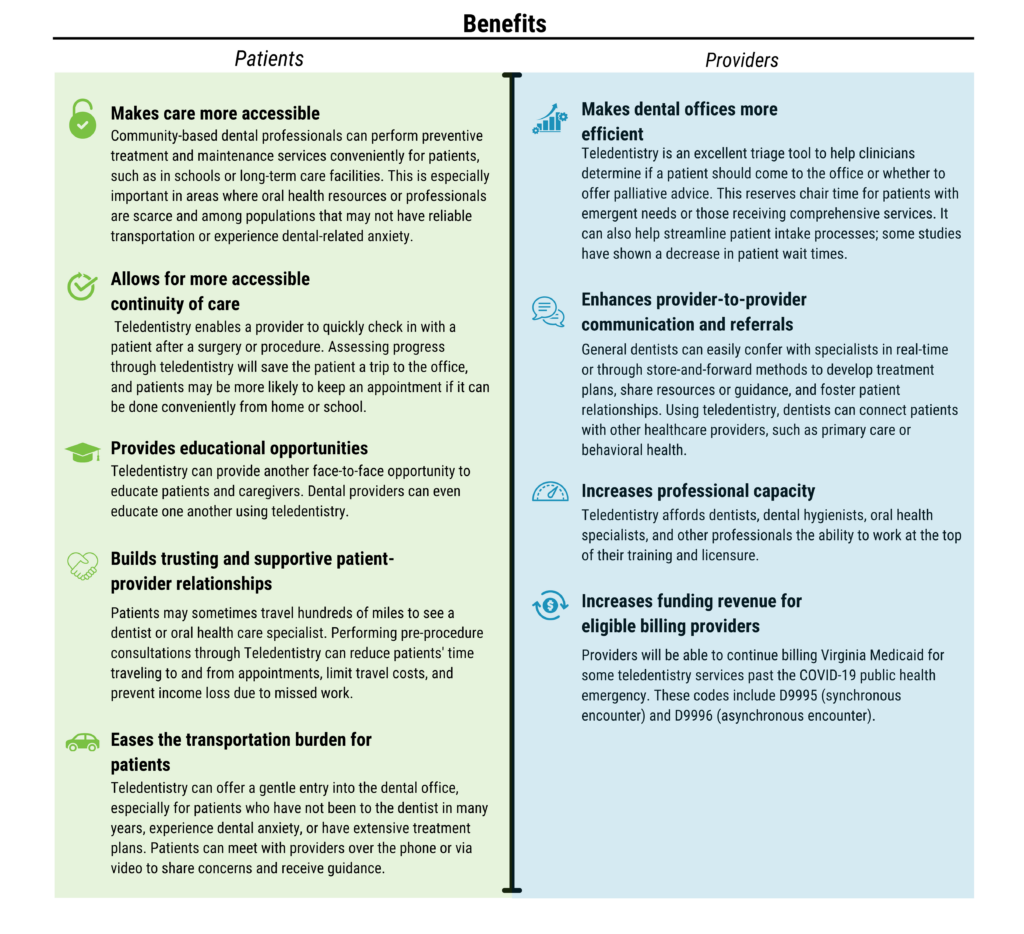
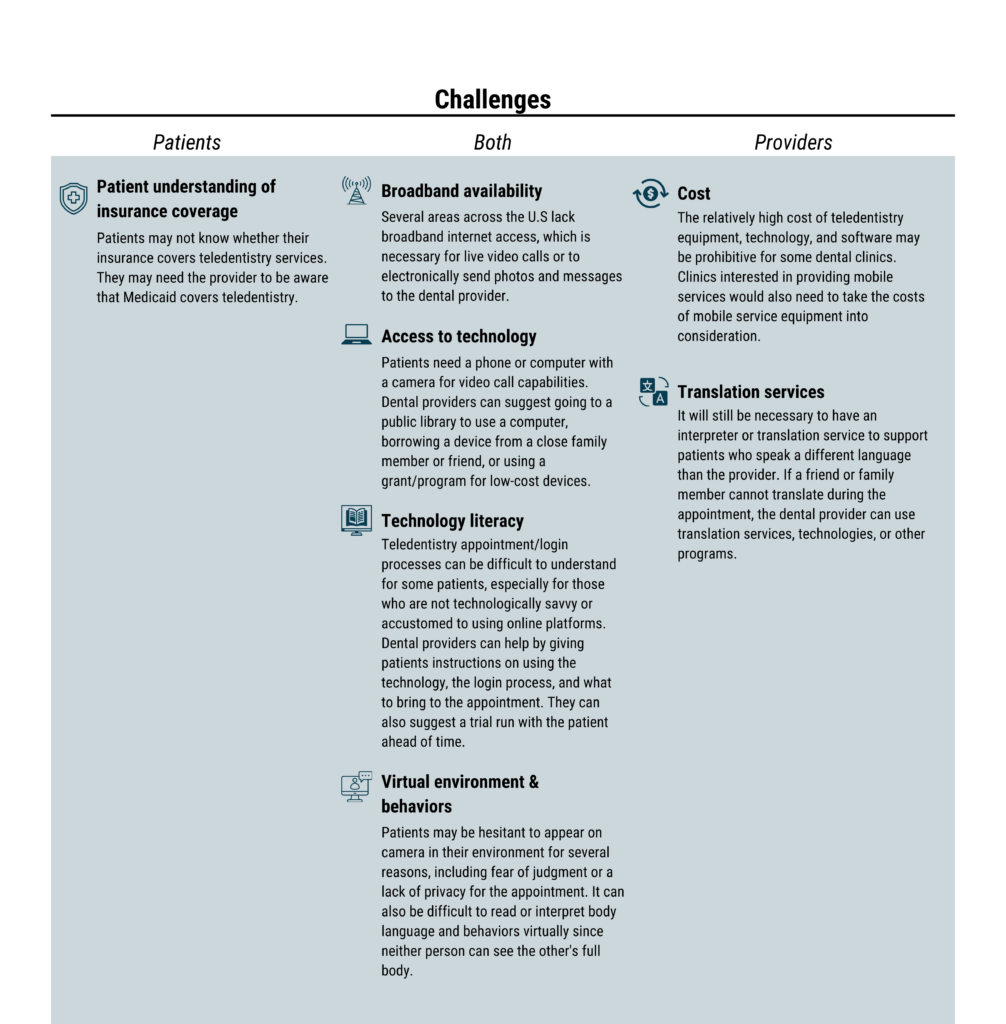
Working within schools as a place of care provides a unique set of challenges and opportunities. School partnerships offer many opportunities that offset potential challenges. When a student leaves the school for an oral health appointment, there are disruptions to regular school attendance. Providing care in the school setting makes it convenient for students and their guardians. Teledentistry delivers care within the school setting to increase access to oral health services for students who might not otherwise have access to dental care or a dental home. These visits help foster connections between provider, patient, and guardian, helping increase the chance of future follow-up visits and addressing the transportation barriers that limit care in the first place.
Logistic and administrative hurdles may arise when navigating the school environment. Parties within the school may have conflicting opinions on the importance of the work or be concerned about how their workload will be affected by integrating into a new program. Common challenges include but are not limited to coordinating school schedules and priorities, managing lines of communication, collecting consent forms, working with and advising families and guardians, addressing privacy, and clarifying specific roles and responsibilities.
Teledentistry in Schools
School-based teledentistry can reduce dental-related emergency room visits and increase access to oral health services, especially for rural patients. Reducing barriers to care, such as transportation and missed school time, supports equitable access to care and improved oral health outcomes.
Using teledentistry to improve access to oral health services in areas with inadequate general and specialty dental care is emerging as a practical solution, especially for treatment planning and specialty consultations. A review of the scientific literature on teledentistry found it to be a promising and effective strategy for increasing access to services in rural and urban areas[i]. Research shows that teledentistry can improve access to oral healthcare and lower care costs [ii].
One study from the CareQuest Institute for Oral Health shows that the average annual dental cost per patient was $75 less for patients with at least one teledentistry visit compared to those who did not have a teledentistry visit in 2018 [iii]. Teledentistry is also an effective way to triage patients. In most instances, teledentistry offers an interactive gateway to appropriate follow-up care. According to the CareQuest Institute for Oral Health, 84% of teledentistry patients had an in-person, post-teledentistry visit within the calendar year, and 71% received in-person care within a week. Only 1% of those patients returned for an emergency visit. The ability to triage using teledentistry allows patients greater access and enables providers to schedule emergency visits more effectively. As clinics utilize teledentistry more regularly, reports show that providers and patients become more comfortable, thus increasing access and cost benefits.
- Six Things to Consider Before Conducting a Teledentistry Visit (Virginia Health Catalyst): Teledentistry visits are different from in-person visits and have specific standards and expectations. Use the tips here to put your patient at ease and ensure a successful visit:
- Teledentistry (CareQuest): The CareQuest Institute for Oral Health has published numerous studies around teledentistry and its benefits. Learn more about their findings and the future of teledentistry on their site.
- Teledentistry Is an Effective Tool to Triage Patients & Save Money CareQuest): Teledentistry can be a cost-effective, low-barrier method to care for individuals. When it comes to triaging patients, patients and clinics can save around 10% of the cost compared to a non-teledentistry visit.
- Fast-Track to Teledentistry: Removing Barriers While Maximizing Overall Health (CareQuest): Teledentistry helps close the gaps in oral health care created by transportation barriers and costs while helping address the oral health workforce shortage. Eliminating these gaps helps providers reach patients earlier in the disease cycle, helping manage conditions before a serious emergency occurs.
- Teledentistry User Guide (NNOHA): The National Network for Oral Health Access (NNOHA) is one of the country’s largest networks of oral health providers. Look at their user guide to learn more about their user models and promising practices.
- Teledentistry website (ATSU School of Dentistry & Oral Health): A.T. Still University’s Arizona School of Dentistry & Oral Health teledentistry site provides resources for patients, oral health providers, educators, and students. While primarily discussing synchronous teledentistry, their resources are suitable for anyone liking to educate their staff, partners, and patients on teledentistry:
- Case Studies of 6 Teledentistry Programs: Strategies to Increase Access to General and Specialty Dental Services (Oral Health Workforce Research Center): Each patient’s contextual conditions will be different when receiving teledentistry services. The University at Albany’s School of Public Health looks at six different cases to highlight how environmental facilitators, barriers, provider attitudes, and technology all play a role in teledentistry implementation.
- Using Teledentistry to Provide Care for Children: The tip sheet – Brush Up on Oral Health for Head Start staff shares basic information about how teledentistry works, using teledentistry in public health settings, the benefits of using it in Head Start programs, and tips for getting started.
This project is supported in part by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services as part of a Health Resources and Services Administration Oral Health Work Force Grant awarded to the Virginia Department of Health (Project Period 09/01/2022 – 08/31/2026). The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government.