Toolkit to increase Well-Child Visits and Vaccinations in School-Aged Youth
The COVID-19 pandemic placed immense stress and risk on our communities, schools, families, and youth in unexpected ways. The pandemic has further highlighted the significant inequities within our communities, particularly access to quality healthcare for our most vulnerable populations. The Centers for Medicare and Medicaid Services (CMS) explicitly report the significant drop in routine childhood immunizations and the gap in immunization rates for those with limited access to private insurance or public insurance.
COVID-19 disrupted in-person learning and routine well-child visits for many children over the last year. As a result, too many children have fallen behind on receiving recommended immunizations. We all want our kids to be back in school safely, which means catching them up on missed immunizations.
 School-based health centers (SBHCs) serve some of the most vulnerable individuals nationwide, reducing barriers such as cost and lack of insurance. By administering immunizations and ensuring youth have an annual well-child visit, either directly or through the coordination of school located vaccination clinics (SLV), school-based health care can further increase access to care, particularly for those youth from families that would traditionally not have any other option for healthcare. Too many children experience persistent disparities in healthcare access, quality, and outcomes. Hence, as a community, we need to support our most needy families to protect them as they go back to in-person learning and begin to feel a sense of normalcy. Centers for Disease Control (CDC) and the American Academy of Pediatrics (AAP) suggest every child continues to receive recommended immunizations during the COVID-19 pandemic. Catch-up immunizations will require efforts from healthcare systems, healthcare providers, schools, state and local governments, and families.
School-based health centers (SBHCs) serve some of the most vulnerable individuals nationwide, reducing barriers such as cost and lack of insurance. By administering immunizations and ensuring youth have an annual well-child visit, either directly or through the coordination of school located vaccination clinics (SLV), school-based health care can further increase access to care, particularly for those youth from families that would traditionally not have any other option for healthcare. Too many children experience persistent disparities in healthcare access, quality, and outcomes. Hence, as a community, we need to support our most needy families to protect them as they go back to in-person learning and begin to feel a sense of normalcy. Centers for Disease Control (CDC) and the American Academy of Pediatrics (AAP) suggest every child continues to receive recommended immunizations during the COVID-19 pandemic. Catch-up immunizations will require efforts from healthcare systems, healthcare providers, schools, state and local governments, and families.
The target audiences for this toolkit are district/school administrators, superintendents, school-based healthcare staff, and community–based healthcare organizations, including staff from state and local public health departments, community health centers, pharmacies, pediatric practices, and health systems.
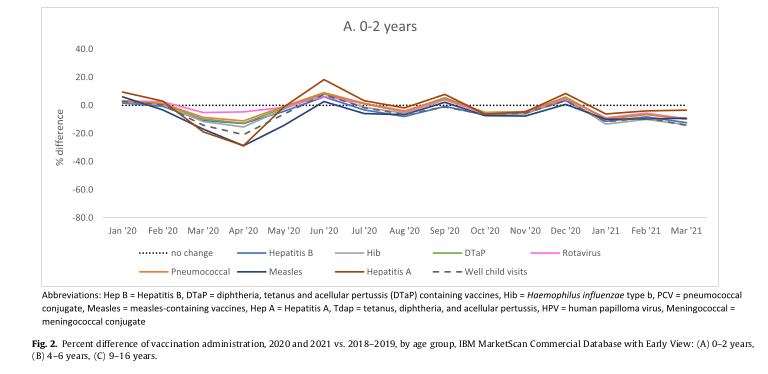
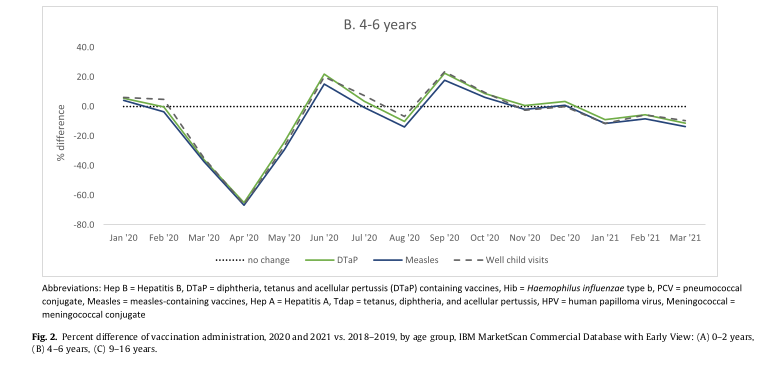
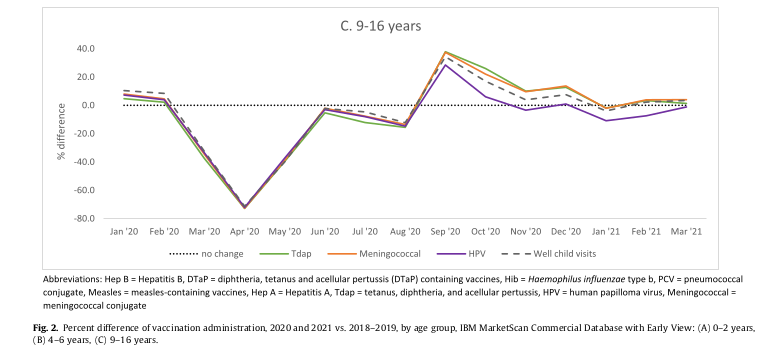
 The JAMA Pediatrics study found that immunization rates were significantly lower across all pediatric age groups as the pandemic first surged in the US. The proportion of those who were up to date on their routine immunizations was lower for most age groups in September 2020 compared to September 2021, and coverage also varied significantly by race and ethnicity. Overall, only 74% of infants under 7 months were up to date on their immunizations in 2020, an 81% drop from 81% in 2019. Only 57% of 18-month-old infants were up to date in 2020, which is 61% down from 2019. The proportion of children who were up to date on immunizations were lowest among black youth. This is relevant information for our school districts, because disruptions to the timing of immunization appointments in early infancy can lead to substantial delays in completion of immunization series as youth enter the school systems, because of the required minimum intervals between immunization doses and the need for additional health care visits to receive missed immunizations.
The JAMA Pediatrics study found that immunization rates were significantly lower across all pediatric age groups as the pandemic first surged in the US. The proportion of those who were up to date on their routine immunizations was lower for most age groups in September 2020 compared to September 2021, and coverage also varied significantly by race and ethnicity. Overall, only 74% of infants under 7 months were up to date on their immunizations in 2020, an 81% drop from 81% in 2019. Only 57% of 18-month-old infants were up to date in 2020, which is 61% down from 2019. The proportion of children who were up to date on immunizations were lowest among black youth. This is relevant information for our school districts, because disruptions to the timing of immunization appointments in early infancy can lead to substantial delays in completion of immunization series as youth enter the school systems, because of the required minimum intervals between immunization doses and the need for additional health care visits to receive missed immunizations.
 It is key to note that immunization rates for routinely recommended immunizations have historically been low in our most underserved, minority communities. The COVID-19 pandemic has only exacerbated the problem.
As related to well child visits, a recent Centers for Medicare & Medicaid Services (CMS) report shows worrisome downtrends in health care utilization during the COVID-19 pandemic for the nearly 40 million children enrolled in Medicaid and the Children’s Health Insurance Program (CHIP).
It is key to note that immunization rates for routinely recommended immunizations have historically been low in our most underserved, minority communities. The COVID-19 pandemic has only exacerbated the problem.
As related to well child visits, a recent Centers for Medicare & Medicaid Services (CMS) report shows worrisome downtrends in health care utilization during the COVID-19 pandemic for the nearly 40 million children enrolled in Medicaid and the Children’s Health Insurance Program (CHIP).
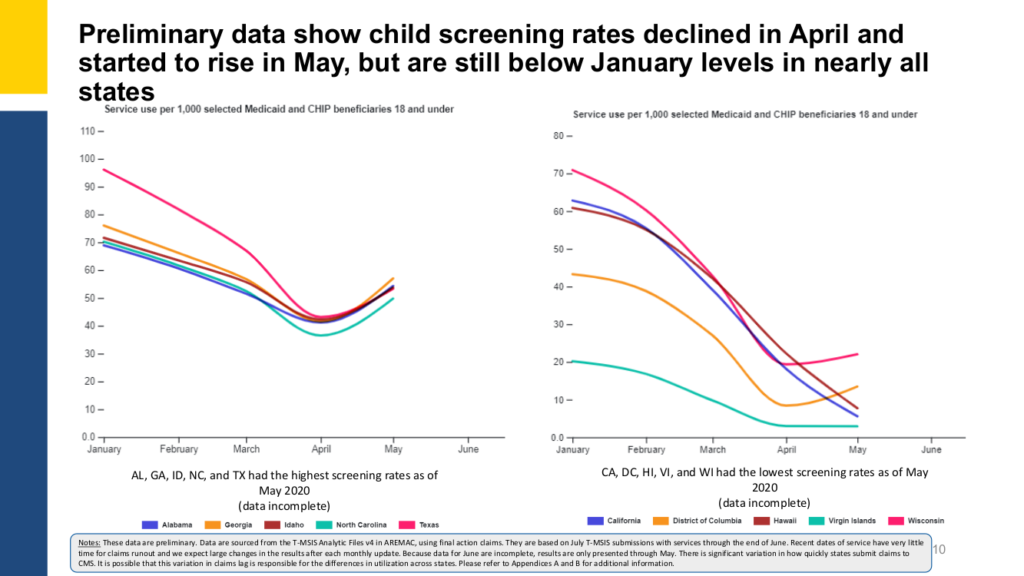
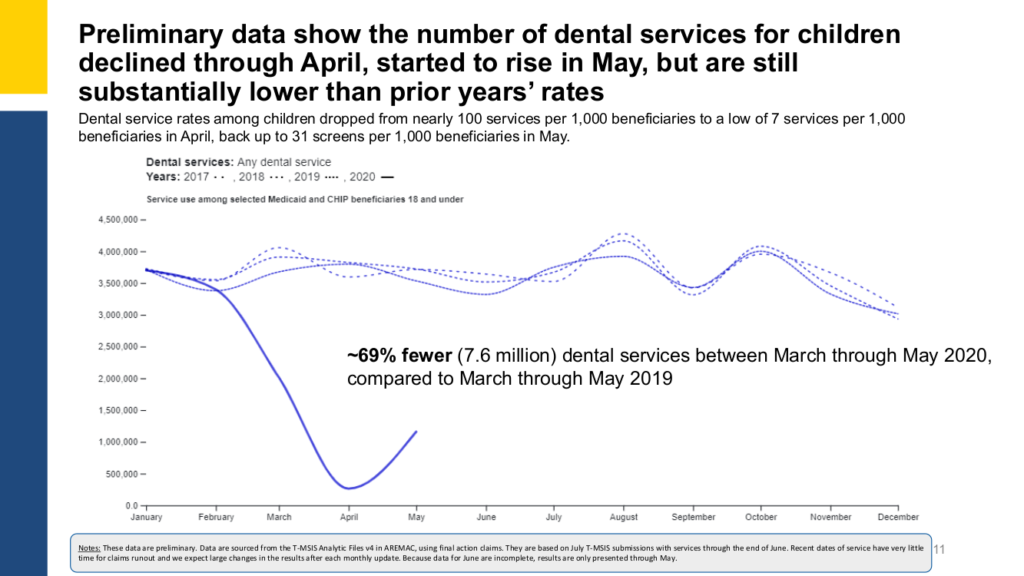
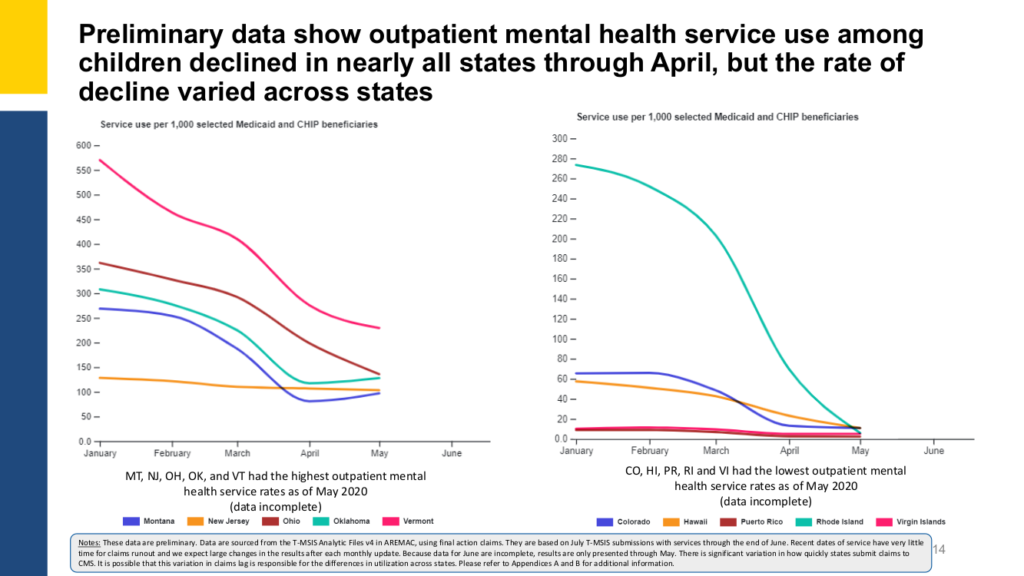 Data reflect a sharp decline in children’s engagement in both primary and preventive care, driven by stay-at-home orders in states across the nation. For children, particularly those from low-income households, the lack of primary and preventive health services can potentially impact physical health, as well as mental health, social-emotional development, and academic outcomes.
Data reflect a sharp decline in children’s engagement in both primary and preventive care, driven by stay-at-home orders in states across the nation. For children, particularly those from low-income households, the lack of primary and preventive health services can potentially impact physical health, as well as mental health, social-emotional development, and academic outcomes.
 Routine well child visits and immunizations are one of the best ways to ensure that kids can return to school successfully and engage in the parts of life that students love –playing with friends, participating in sports, and connecting with their teachers. Well-child visits are an opportunity for parents to support the whole child, both their physical and behavioral wellbeing. Caregivers can ask questions about nutrition and safety and their child can be screened for developmental delays or behavioral and mental health concerns.
Routine well child visits and immunizations are one of the best ways to ensure that kids can return to school successfully and engage in the parts of life that students love –playing with friends, participating in sports, and connecting with their teachers. Well-child visits are an opportunity for parents to support the whole child, both their physical and behavioral wellbeing. Caregivers can ask questions about nutrition and safety and their child can be screened for developmental delays or behavioral and mental health concerns.
 Immunizations not only protect the individual receiving the immunization, but also the community preventing the spread of these diseases. While there are no federal laws regarding the requirement of immunizations, all 50 states have legislation requiring children attending public school to be vaccinated against diphtheria, tetanus, and acellular pertussis (DTaP); polio (IPV); measles and rubella (MMR); and varicella (chickenpox). All states and the District of Columbia, however, allow medical exemptions for children who have a medical condition preventing them from receiving an immunization.
Immunizations not only protect the individual receiving the immunization, but also the community preventing the spread of these diseases. While there are no federal laws regarding the requirement of immunizations, all 50 states have legislation requiring children attending public school to be vaccinated against diphtheria, tetanus, and acellular pertussis (DTaP); polio (IPV); measles and rubella (MMR); and varicella (chickenpox). All states and the District of Columbia, however, allow medical exemptions for children who have a medical condition preventing them from receiving an immunization.
 Schools and healthcare providers have an opportunity and responsibility to advance health equity and assure that every child has a fair chance to reach their potential. During the pandemic, African American and Latinx/Hispanic children missed well-child visits at rates greater than their white counterparts (33% and 35%, compared to 27%, respectively). We all have an opportunity to do better. Our public health partners and local community organizations can all play a part in reaching families with the services that they need.
Schools and healthcare providers have an opportunity and responsibility to advance health equity and assure that every child has a fair chance to reach their potential. During the pandemic, African American and Latinx/Hispanic children missed well-child visits at rates greater than their white counterparts (33% and 35%, compared to 27%, respectively). We all have an opportunity to do better. Our public health partners and local community organizations can all play a part in reaching families with the services that they need.
 These are challenging times, but we have the power to help our youth and families. Working together, schools and healthcare providers to bring high quality healthcare to our youth and ensuring they receive an annual well-child visit and recommended immunizations is one of the best things you can do to protect your child and community from serious diseases that are easily spread. The health care of our students is a national priority, and school-based health care plays a critical role in this goal. Youth are more likely to succeed educationally if they are healthy and in school.
Caregivers/guardians, educators, and healthcare workers all want the best for children and adolescents. Positive health outcomes support improved educational outcomes by reducing or eliminating nonacademic barriers to learning.
These are challenging times, but we have the power to help our youth and families. Working together, schools and healthcare providers to bring high quality healthcare to our youth and ensuring they receive an annual well-child visit and recommended immunizations is one of the best things you can do to protect your child and community from serious diseases that are easily spread. The health care of our students is a national priority, and school-based health care plays a critical role in this goal. Youth are more likely to succeed educationally if they are healthy and in school.
Caregivers/guardians, educators, and healthcare workers all want the best for children and adolescents. Positive health outcomes support improved educational outcomes by reducing or eliminating nonacademic barriers to learning.- School-based healthcare programs represent a partnership between schools and community health organizations. Their objective is to give students meaningful access to care in a safe and convenient location. Whether onsite, mobile, or through telehealth, various healthcare professionals collaborate with schools to address the broad range of concerns and adverse experiences that affect students’ healthy development. These services include acute/chronic healthcare management, primary care, vision/dental, mental/behavioral health, and preventive care. Some programs serve only students, while others serve family members and the school’s broader community. Programs offer a range of services, with the most common being primary medical services. School-based health programs respond to local needs, receive support from many communities, and are as individual as the clients they serve. No matter the configuration, the team brings its expertise, resources, and authority to improve students’ physical, social, emotional, and behavioral health. School-based healthcare is a powerful tool for achieving health equity among children and adolescents who unjustly experience disparities in outcomes simply because of their race, ethnicity, or family income. Visit School-Based Health Centers and School Nurses to learn more about school-based health programs.
- Immunizations are physical interventions used to stimulate the body’s immune response against diseases. The administration of immunizations usually occurs via a needle injection and sometimes by mouth or nasal pathways.
- A well-child visit is a routine medical visit for comprehensive preventive healthcare services. It typically occurs annually from infancy to age 21. Services include a risk assessment, physical exam, measurements, vision and hearing screening, an oral health risk assessment, health guidance or counseling, and ensuring that all required and recommended immunizations are up to date.
School/District Administrators
School/District Administrators
Learn MoreCommunity Healthcare Providers
Community Healthcare Providers
Learn MoreSchool Nurses
School Nurses
Learn MoreGeneral Resources
General Resources
Learn MoreBest Practice Case Studies
Best Practice Case Studies
Learn MoreThe National School-Based Health Alliance developed this toolkit in collaboration with our valued partners: The National Association of School Nurses (NASN) and The School Superintendents Associations (AASA). We sincerely thank both NASN and AASA for their continued partnerships, providing valuable information for the toolkit, and for supporting our schools and school-based health programs across the country. We collectively want to thank all school-based health program providers and staff for their hard work and dedication to ensure our youth and families have access to quality healthcare. We also gratefully acknowledge the Merck Company Foundation for providing the financial support for this project.