Starting an HCT Process
The Playbook guides SBHCs and other school staff on assisting students with their preparation for the transition from pediatric care to adult health care. Guidance and sample resources can be found in the following Playbook sections: Starting an HCT Process, HCT Intervention Tools, Examples from the Field, and Additional HCT Resources.”
Form a Team and Enlist School Support
Purpose: Implementing lasting changes in your SBHC will require a strong, effective, and dedicated team. Select the members of your team for their ability to influence, create, or change the policies and practices necessary to support your HCT Intervention. Cultivating this team will require a solid and enthusiastic team leader. See pages 4-5 in Got Transition’s Implementation Guide for more information.
Steps:
- Secure Leadership Support
- Gaining the support of the SBHC and other school leaders to develop and implement long-range goals will allow your team to move from planning to full implementation. Be prepared to make a case for why HCT is important (see “Why do Adolescents need Health Care Transition Guidance?”) and how you plan on implementing HCT services with your students.
- Leadership support will help the following:
- Backing the project publicly and actively
- Aligning with other strategic activities
- Ensuring dedicated time for the team to pilot the HCT intervention
- Ensuring availability of resources, such as health information technology
- Endorsing/guiding expansion from the pilot phase to full implementation
- Communicating with other leaders and stakeholders in the school or organization sponsors when needed
- Form Your HCT Team
- Your HCT team should reflect the diversity of your SBHC and students. It works best to include representatives from all areas of your SBHC (e.g., medical and mental health providers, health educators, outreach workers, front office staff, and students). Consider including other school-based team members such as school nurses, school counselors, and special education leads.
- Bring Team Members Together
- Have an initial meeting to introduce the contents of this School HCT Playbook, including the sample tools. Schedule subsequent regular meetings, decide who will keep minutes, establish roles, and have team members report progress regularly.
Considerations:
- On day one, establish roles and responsibilities for all team members!
- A team diverse in gender, race, cultural background, and sexual identity will generate more support and engagement.
- Include student representatives (at least two) to voice their peers’ input and ideas.
- Keep the size of your team manageable.
- If you’ve done Quality Improvement work before, build on a former/existing team to help your HCT Team.
Additional Resources:
Develop an HCT Improvement Plan
Purpose: Tracking and monitoring your HCT program’s implementation and success is essential to ensuring its sustainability. Starting with a clear goal and subsequent milestones will help you track progress and spot any potential barriers or pitfalls along the way. See pages 6-7 in Got Transition’s Implementation Guide for more information.
 Steps:
Steps:
- Baseline assessment
- Begin by assessing where you are in terms of HCT implementation using Got Transition’s Current Assessment of HCT Activities for SBHCs. Complete the assessment annually to document changes and improvements.
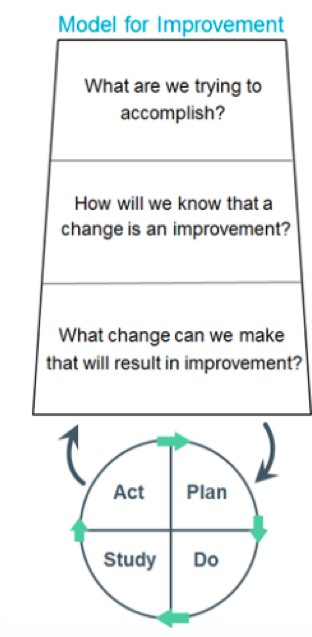
- Implement an Improvement Model Approach by answering these three questions:
- What are we trying to accomplish?
- Develop an objectives statement that describes the improvement effort and includes the rationale for doing the work, the target population, period of work, and measurable goals.
- Start with a clear vision and definition of success to enable you to act intentionally and proactively throughout the implementation.
- Example objectives statement: Understanding why transition from pediatric to adult care is vital for students leaving high school. By (date), we will co-produce (with students) a welcome and care policy/guide, and by (date), 90% of students will receive it during their SBHC visit, with documented receipt in their medical record.
- Start with a clear vision and definition of success to enable you to act intentionally and proactively throughout the implementation.
- Develop an objectives statement that describes the improvement effort and includes the rationale for doing the work, the target population, period of work, and measurable goals.
- How will we know that a change is an improvement?
- Example: Documentation in the medical record that the welcome and care policy was shared with students coming for preventive care visits.
- What changes can we make that will result in improvement?
- The structured HCT process you are implementing improves health outcomes. (see Why Do Adolescents Need HCT Guidance #4)
- What are we trying to accomplish?
- Plan how to implement the dissemination of the welcome and care policy.
- Create a system (e.g., SBHC front desk staff reminder) to ensure the sharing of the welcome and care policy with students at preventive care visits.
- Choose and review the SBHC HCT tools you want to implement
- Choose tools you want to implement and customize if needed. Use Plan, Do, Study, Act (PDSA) cycles with 3-4 students who review the customized tools and validate their understanding of the content.
Considerations:
- Consider your intended population, scope, and timeline in your objectives statement.
- Who is your intended population? Do you intend to focus on juniors and seniors or all high school students? What about other special populations?
- Do you intend to include students with Individual Education Plans (IEPs)? If so, consider collaborating with special education teachers, social workers, etc.
- Do you intend to include students with mental/behavioral health needs? If so, consider collaborating with other school-based providers.
- How are you tracking progress? Ideally, use measurement tools frequently during the implementation (see section Develop an Implementation Plan/Workflow)
- How are you training SBHC staff on HCT?
- Do you intend to coordinate your SBHC HCT efforts with other providers seen by individual students outside of the school?
- How will students find adult providers (e.g., primary care, mental health) or community resources after they no longer use the SBHC?
Additional Resources:
Develop an Implementation Plan/Workflow
Purpose: Create a workflow to hardwire HCT tools and processes into your SBHC. It should involve examining all the actions required, people involved, and decision points along the way.
Steps:
- Create a workflow or flow map:
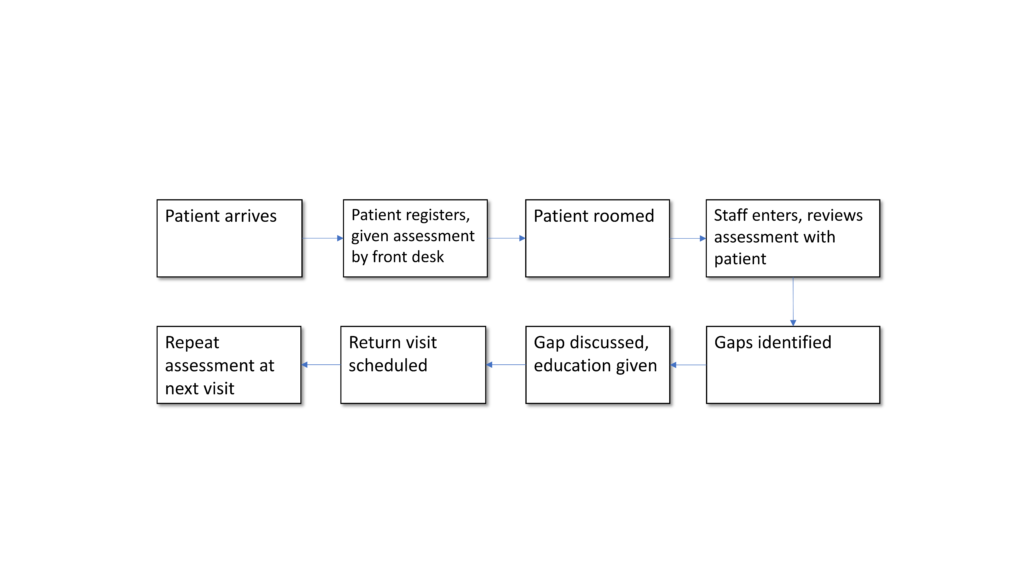
- Use the HCT tools to create and implement a workflow or flow map that embeds HCT into your SBHC routine.
- A flow map visually displays the separate steps in a process placed in sequential order. It is conducive to documenting different views of the same process. It can show the sequence of actions, materials/inputs entering and leaving the process, decision points, and people involved. Flow maps can document either how things are or how things could be. Posting the flow map allows staff to clarify the steps in the process and can uncover conflicts in understanding.
Example:
- Plan, Do, Study, Act (PDSA) Cycles
- Try small tests of change through PDSA cycles to see if your process works in your SBHC.
- Test your tool/process with 3-4 students over the next 2-3 days.
- Increases belief that change leads to improvement
- Helps to adapt ideas/tools to your SBHC workflows
- Predicts problems from planned change
- Minimizes clinic resistance
- Monitors your workflow
- Revisit this workflow several times throughout the first year to ensure you are reaching all targets and meeting all goals.
Considerations:
- Who needs to be involved in the HCT program, and in what capacity?
- Educate all team members about the process.
- Create a written document to describe the clinic’s approach to implementing the process.
Additional Resources:
Track and Measure HCT Improvements
Purpose: Tracking and measuring the HCT improvement intervention allows for data-driven decision-making. The following steps are several ways that SBHCs can track and measure HCT success.
Steps:
- Tracking system: Establish criteria and a process for identifying the student population to be served by the HCT intervention and a method to track receipt of the HCT intervention through an excel registry (see the example from a pediatric practice).
- Assessment of HCT implementation: At the outset of the pilot, conduct a Current Assessment of HCT Activities to determine the baseline level of HCT implementation within the SBHC. Perform the assessment annually to measure process improvements.
- Student Feedback: Typically conducted with seniors who have received HCT services, this example of a brief survey, used in pediatric practices, offers an opportunity to discover what the student’s experience has been with the SBHC’s HCT services, how prepared they felt to move to an adult doctor, and suggestions for improving the HCT process.
Considerations:
- Tracking system:
- What population will you include in your tracking and monitoring (e.g., demographic, medical/social complexity, and date of receiving the HCT services offered)?
- What tracking format will be used?
- Will you need to put this tracker into your electronic medical record?
- Who will input the information?
- Assessment of HCT Implementation:
- Find a time when clinic and administrative staff are meeting and complete the Current Assessment Tool before the start of HCT intervention.
- This self-assessment can help build an objectives statement.
- Student Feedback:
- How will student anonymity be protected while gaining their feedback?
- When will the survey be given (e.g., to all seniors who used the SBHC or to seniors following their last preventive visit)?
Additional Resources:
Communicate, Disseminate, and Advocate
Purpose: Your HCT program needs the support of your SBHC, as well as engaged stakeholders within the school, organizational affiliates, and the student body. See pages 9-10 in Got Transition’s Implementation Guide for more information.
Steps:
- Communicate the Need
- There is clear evidence that most students have not received anticipatory guidance from their health care providers about HCT. Most feel unprepared for adult health care. Thus, SBHCs are filling a critical unmet need. See Introduction for more.
- To gain traction, ongoing advocacy within and outside of your SBHC will be vital for generating buy-in.
- Communicate the Success:
- Communicate five times, five different ways.
- Share your implementation progress, the gains you are making with your HCT objectives statement, the roadblocks you have overcome, and the feedback from students and clinicians alike, using the measurement tools previously discussed.
- Celebrate Progress Regularly:
- Reward this work at staff and team meetings.
- Display posters in the waiting room explaining the project.
- Have the SBHC participate in a learning collaborative with other SBHCs.
- Share your work with a practice improvement committee, district-wide meeting, or conference.
- Plan for Sustainability/ Spread:
- After six months, revisit your processes and goals.
- Aim to hardwire your program into the SBHC by including HCT activities into job descriptions so when staff turns over, the HCT process continues.
- Train all SBHC staff to use the HCT tools and consider creating a sustainability plan.
Considerations:
- How are you communicating regularly with the rest of the SBHC, school, and other organizational leaders?
- How are you communicating about HCT to students in the school as a whole? What about communicating with parents?
- Try using multiple modes of communication (e.g., brochures, presentations at school meetings, graduation preparation talks, posters).
Additional Resources: