Preparing for Implementation
Click the below icons to read more about each topic
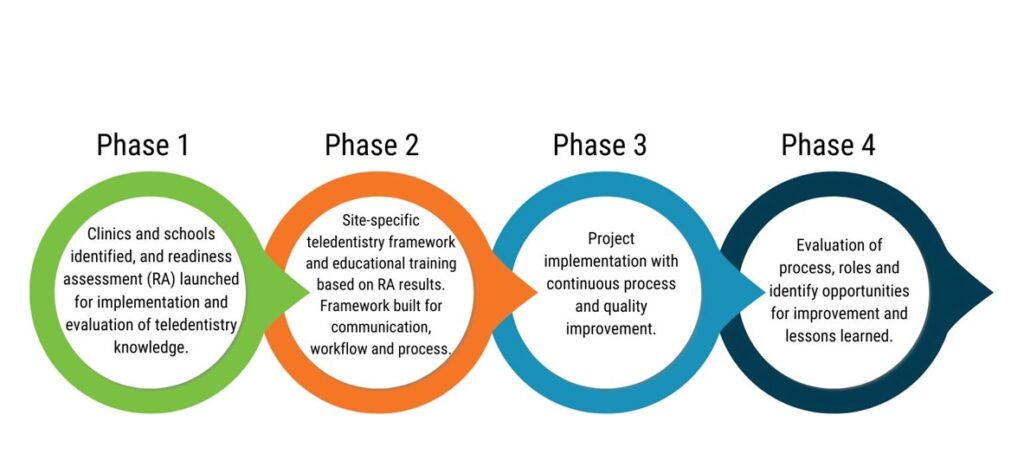
Teledentistry can be employed and is proven beneficial for oral health promotion, education, diagnosis, and monitoring of oral health conditions. Given the unique aims of teledentistry implementation, there is not one design that fits every program. Each team will design their program based on their unique capacities and readiness. Once a team establishes the foundations of the program and an initial process map or workflow, the improvement opportunities do not end. A future state process map or workflow will help manage the changing environment and is part of ensuring continuous quality improvement.
Assessing Readiness
A School-Based Teledentistry Readiness Assessment (SBTRA) helps to understand the readiness of the clinic team participants to build a school-based teledentistry program. Through the process of creating an infrastructure for a new initiative, it is essential to understand the knowledge and readiness of each person to implement teledentistry.
The readiness assessment establishes baseline and outcome measures to help build out project learning modules. Based on the readiness assessment results, you can inform future oral and integrated healthcare educational opportunities and areas needing attention to improve processes and students’ overall health. The Catalyst team created the Virginia SBTRA tool based on staff and external clinical experience and expertise. The results from the SBTRA provide insights into what technical assistance, education, and resources regarding teledentistry implementation and sustainability the participants will need.
Catalyst staff developed education tools and training modules based on identified gaps from the SBTRA and the implementation of best practices. The readiness assessment also identifies possible implementation challenges with new procedures or processes for each team.
School-Based Teledentistry Readiness Assessment Overview
- Assesses people’s capacity, including staff’s knowledge, skills, and motivation to adapt to change.
- Assesses organizational capacity, including structures for system change, internal communication, and establishing clear roles and responsibilities.
Considerations:
1. When building your assessment, ask: What is the goal of your teledentistry program?
2. Be specific. Include patient populations and measurable outcomes.
3. Design a workflow and process map as a team.
4. What specific tasks does each staff member get assigned? Think from start to finish – scheduling the appointment through follow-up.
- Who will collect patient/caregiver consent?
- How will the appointment be scheduled?
- Who needs to be present for the appointment?
- Who will record the notes and track the next steps?
- If asynchronous, when will patient photos be reviewed?
- How will you train dental and medical staff in the new technology?
- Who needs to receive training?
- How will you provide technology-related education and assistance to patients?
- How will you follow up with patients? (Via the patient portal, over the phone, via text message, etc.)
- How will you inform patients of the available new teledentistry services? (Social media, mailings, radio ads, billboards, etc.)
Memorandum of Understanding (MOU)
Once a team completes the School-Based Teledentistry Readiness Assessment, they can more clearly communicate with their educational partners and develop a shared agreement on the school-based teledentistry components. A memorandum of understanding is the next step that clearly outlines the partnership’s WHY, WHAT, and HOW.
The memorandum between a healthcare entity and a school formalizes the terms and conditions under which parties will work together to support the provision of specific healthcare services in the school setting. The document is typically not a legal document, although all organizations may seek legal counsel to develop and sign the document. The MOU usually clarifies a cooperative/collaborative arrangement involving two or more organizations, indicating how they will work together, representing the goodwill of each organization, and helping define their expectations, roles, and responsibilities. The MOU addresses such things as the following (not exhaustive but illustrative)
- Foundational written agreement to establish policies and procedures
- Purpose of the collaboration
- Responsibilities of all parties
- Billing and compensation
- Confidentiality
- Termination provisions
- Scope of agreement
- Liability
Consent Forms
Consent is critical to the success of a school-based teledentistry program, allowing the students to seek services when they need them in the school setting. Education partners are vital partners in obtaining consent for services.
Considerations for consent forms:
- Consent forms for the school-based teledentistry program should align with protocols and procedures used in your brick-and-mortar clinic.
- Consent forms should be concise with health literacy in mind, including simple language vetted by the school staff and families and translated based on the patient population.
- Consider adding a Q.R. code and a workflow with the school nurse that includes having multiple ways to share the consent form with the parent/guardian if the child does not have one on file.
Additionally, consider sharing information about the program and consent in the following:
Caregiver newsletters
Open houses
School website and events
Inserts in student folders
Communications from school staff
Defining Services in your Consent Process
- Oral health education and referrals: a professional educates, guides, and refers patients to local dental providers.
- Emergency triage: providers understand the severity of a case to determine the next steps, including scheduling an in-person visit or prescribing appropriate medications.
- Consultations or patient monitoring: save patients a trip to the office and keep the dental chair available for hands-on procedures by conducting pre- and post-surgery consultations through teledentistry.
- Limited oral exam or preventive services: dentists can make initial diagnoses, establish treatment plans, or authorize remote services.
- Community-based comprehensive care (virtual dental home): members of the care team deliver comprehensive oral health services remotely (at school, different clinic locations, long-term care facilities, designated community centers, etc.) through authorization and guidance of providers using teledentistry.
Financial Planning
Understanding the allowable uses of teledentistry in your state and which codes/procedures allow for reimbursement is essential. Working to the top of their license and providing reimbursable services, each staff member influences sustainability. Clinic staff will need to work with their internal billing and reimbursement team to increase accuracy and reimbursement. Clinics must work to diversify their funding streams to ensure sustainability and the flow of under and uninsured students. Example funding streams are listed below:
Medicaid
Private Insurance
Sliding fee scales
Grants and fundraising
In some states, Medicaid school-based services allow school districts to receive partial reimbursement for qualifying health and related services.
- ADA Guidance on Teledentistry Encounters:
The ADA continually issues guidance on Teledentistry encounters and billing around services. For a summary of some of their guidance, you can access this guide from Mouthwatch.
D9995 & D9996: Coding for Teledentistry D9995 & D9996 are two CDT codes utilized for teledentistry and delineating between modalities. For case examples and more information on when to use what codes, look at the Mouthwatch informative guide.
This project is supported in part by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services as part of a Health Resources and Services Administration Oral Health Work Force Grant awarded to the Virginia Department of Health (Project Period 09/01/2022 – 08/31/2026). The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government.